The DHIS2 Annual Conference takes place from 15-18 June 2026! Learn more
Rapid containment of an Ebola outbreak in the DRC with DHIS2
DHIS2 was at the center of the Democratic Republic of the Congo’s response to the 2025 Ebola outbreak, helping health authorities to quickly detect cases, follow up contacts, and coordinate across partners
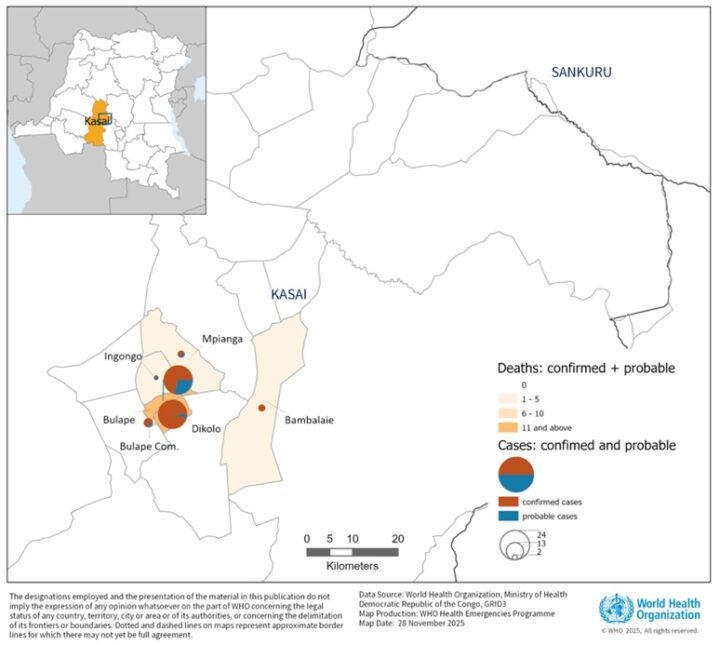
On December 1, 2025, the Ministry of Health (MoH) of the Democratic Republic of the Congo (DRC) declared an end to the country’s 16th reported Ebola outbreak, just under three months after it began. A total of 64 cases were identified, leading to 45 deaths. The declaration was made 42 days after the final person confirmed with Ebola Virus Disease (EVD) was discharged from treatment after testing negative for the virus.
DRC’s success in identifying and controlling the outbreak was thanks to a collaborative effort that included the WHO, the Congolese Red Cross, and other partners, supported by rapid reporting and effective data use through DRC’s national DHIS2 system. Health workers were able to localize the epicenters of the outbreaks and follow up nearly 600 contacts in order to identify cases and prevent further spread of this deadly disease.
As the leader of the Africa CDC’s incident management team explained to Nature Africa:
“Using the DHIS2 platform, adapted for emergencies, patient information from surveillance, laboratory testing, and treatment centres, now feeds into a unified database. Health workers use smartphones to report cases in real-time, enabling immediate contact tracing and vaccination campaigns.”
Ngashi Ngongo — Africa CDC (source)
Digital tools for rapid detection and response
The 2025 Ebola outbreak was declared in early September in the Bulape and Mweka health zones in DRC’s Kasaï province, a hard-to-reach rural area near the border with Angola. As Ebola is a deadly contagious disease—with case fatality rates ranging between 25% to 90% in previous outbreaks—rapid access to reliable and actionable data was critical to help investigate reported cases and control the outbreak’s spread.
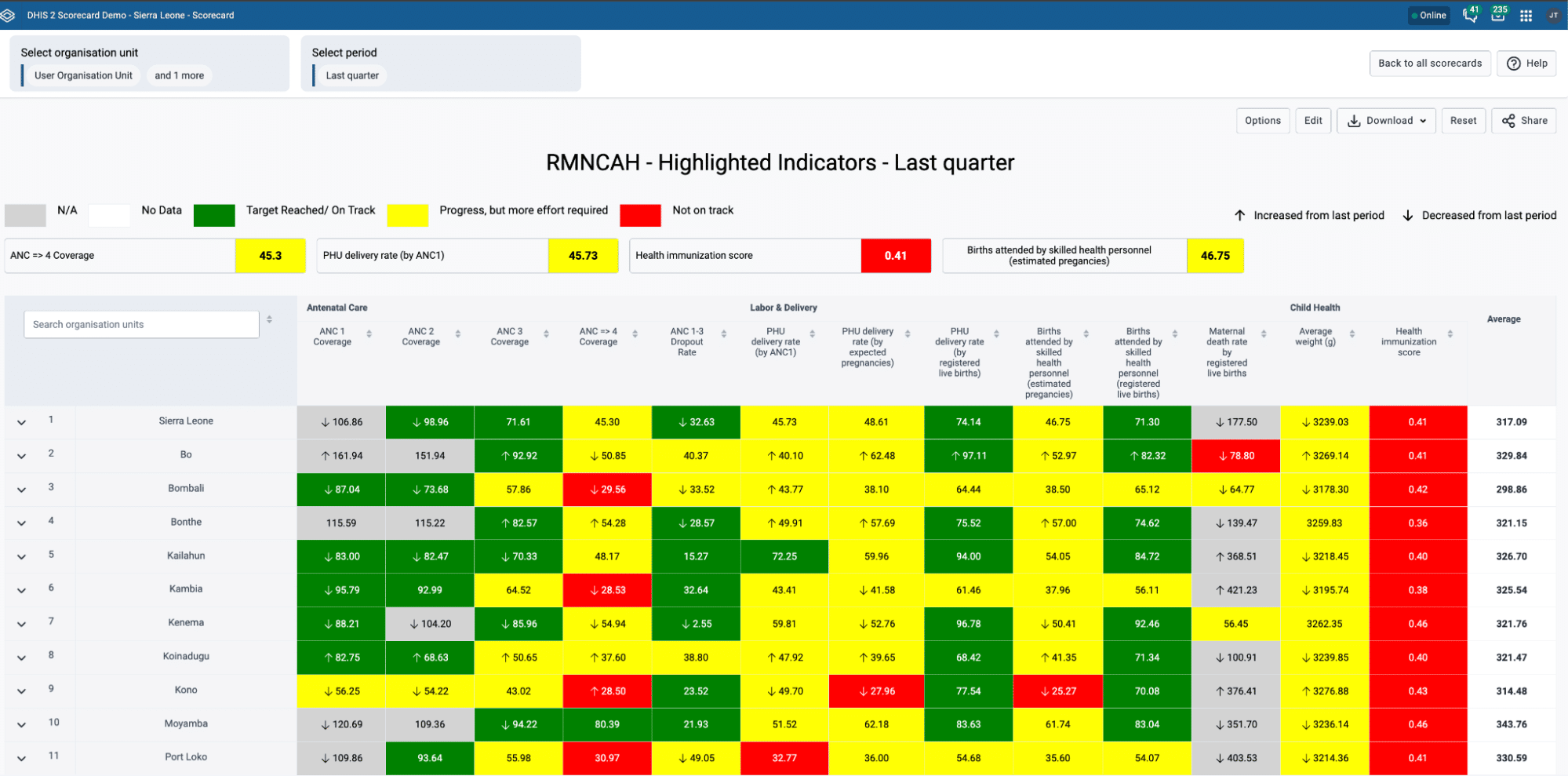
RTI, HISP DRC, and their partners leveraged the country’s national health information system by configuring an EVD tracking tool in DHIS2. The tool included dedicated stages for suspected cases, contacts, laboratory results, case outcomes, and vaccination of contacts and frontline responders, allowing health workers working on different aspects of Ebola response to enter data in one shared system in near real-time.
Response teams and national authorities used DHIS2 analytics and notification tools—including SMS alerts, dashboards, and interactive maps—to monitor the progression of the outbreak and ensure the timely deployment of contact tracing teams and support services to priority locations. DHIS2’s offline data entry functionality enabled health facilities and contact tracing teams operating in remote areas to continue collecting and transmitting data using Android tablets, thereby strengthening outbreak preparedness and response.
This digital approach reinforced the three core pillars of epidemic management:
- Detect: By digitizing case-based surveillance, the DHIS2 Tracker enabled the rapid identification of suspected Ebola cases and their contacts, providing health authorities with near real-time visibility of potential transmission chains.
- Notify: The system automatically captured and shared data with national authorities, generating timely alerts for suspected and confirmed cases. This reduced reporting delays and strengthened compliance with Integrated Disease Surveillance and Response (IDSR) reporting requirements.
- Respond: Supported by analytical dashboards and workflows for contact tracing and laboratory results management, the tracker helped response teams prioritize follow-up visits and allocate resources more effectively. This targeted approach accelerated case management for confirmed cases and contributed to the containment of transmission.
An article on the outbreak published by RTI notes how the Ministry of Health and their partners worked together to put DHIS2 “at the center of the response”:
“That single alert sets off a chain: contacts to visit, homes to reach. A specimen is collected, given a unique ID, and tracked like a relay baton to the lab. Results flow seamlessly into DHIS2. Vaccination data joins the stream. And from a command dashboard, incident managers zoom from a bird’s-eye view of the outbreak down to the doorstep of the one contact still waiting.”
Trudeau, Ngoyi and Gupta — RTI International (source)

Facilitating concrete impact: Faster test results and better oversight
The report from RTI notes several key impacts that were achieved through the use of DHIS2 for EVD outbreak response:
- Faster notification of lab testing results due to reduced time from specimen collection to results, as data for every stage of the process is directly entered and tracked in DHIS2, making it available in near real-time.
- Better targeting of contact follow-up as the command center staff can quickly see which contacts have not yet been visited and deploy teams to close the gaps.
- Improved data reliability thanks to routine checks for reporting timeliness, completeness, and accuracy that help ensure data quality.
- Verifiable certification of discharge for previously infected patients, featuring a scannable QR code linked to their DHIS2 record, helping to counteract the stigma that is often associated with Ebola infection.

Leveraging existing infrastructure and local capacity
The “backbone” of the DRC’s Ebola response was the country’s existing, locally owned and managed DHIS2 infrastructure. The DRC was already using DHIS2 for disease surveillance before the 2025 EVD outbreak began, as part of an ongoing project to digitalize their surveillance systems nationwide. National health authorities have used this system to monitor and respond to several disease outbreaks, including for mpox surveillance and vaccination activities with support from Gavi, Africa CDC, and HISP DRC. HISP has also previously worked with health and agriculture authorities in the DRC to pilot system for animal health and zoonotic disease surveillance.
Beyond disease surveillance, the DRC has used DHIS2 as a national-scale Health Management Information System (HMIS) since 2013, utilizing it for health program planning and management at the zonal, provincial and national levels. This long history with DHIS2 as a locally-owned data platform—which has been supported by funders such as Gavi, the Global Fund, and the CDC and technical partners including HISP, RTI, MEASURE Evaluation (ME) and others—means that the DRC’s Ministry of Health has a solid foundation of digital infrastructure and local capacity, plus a network of long-term partners who can assist in times of crisis.
While HISP researchers in 2022 uncovered some ongoing challenges with DHIS2 data use in the DRC, they also noted that it was to a large extent a “success story,” with clear evidence of stakeholders in the immunization, malaria, and tuberculosis programs using the platform for improved data collection and informed decision making. The DRC’s more recent successes using DHIS2 for vaccination campaigns and disease surveillance and outbreak response illustrate how the country continues to build on this foundation, helping to improve health security and achieve better health outcomes for its population.
Looking ahead: Improving linkages between HMIS, surveillance, and campaign systems
The MoH in DRC has successfully demonstrated the impact of using DHIS2 for rapid outbreak detection, notification and response for recent outbreaks including Ebola and mpox; and how shared infrastructure and local capacity can accelerate the containment of disease outbreaks through a flexible digital platform. Yet, outbreak response databases for different disease outbreaks remain fragmented in DRC and many other countries, and the need to configure DHIS2 Tracker programs to support the specific response needs at the outset of each individual outbreak can lead to alignment challenges with rapidly deployed tools like Excel-based line lists. The development of an integrated, ready-to-use, multi-disease platform thus remains a key goal. Connecting surveillance and routine immunization systems could reduce the potential for data quality issues related to vaccination of outbreak contacts and responders. There are also opportunities to improve linkages with DRC’s routine HMIS, routine IDSR and integrated health campaign systems as part of national architecture so that data is seamlessly shared between systems and stakeholders at all levels.
Looking ahead, DRC is advancing a strategy for establishing a unified surveillance and emergency response system with DHIS2 in partnership with Africa CDC, HISP DRC and HISP UiO. Using lessons learned from DRC’s outbreak response efforts with DHIS2, HISP and Africa CDC will develop shared resources as part of a new toolkit to support countries to implement integrated surveillance and emergency response platforms, enabling the adoption of successful approaches across the African continent.