The DHIS2 Annual Conference takes place from 15-18 June 2026! Learn more
Learning from DHIS2 climate-informed early warning pilots to develop innovative open-source AI tools
Action research by HISP UiO, local HISP groups, and national public health partners in Mozambique and Laos has helped inform the design of the Chap Modeling Platform and our larger approaches to predictive modeling and early warning in the DHIS2 for Climate & Health project.
Climate-sensitive infectious diseases like malaria and dengue post a significant threat to public health, especially in low- and middle-income countries (LMICs). For example, Mozambique is considered by the WHO to be a high-burden country for malaria, with the entire population at risk. Meanwhile, Laos has been facing a significant increase in infections and deaths from dengue since 2023. As changing factors influence the geographic distribution and timing of malaria and dengue outbreaks, digital tools that can enable health authorities to predict changing disease patterns can help them plan more effective–and more cost-effective–interventions, potentially reducing malaria incidence and saving lives.
Mozambique was one of the first countries to explore the use of health data and weather data in DHIS2 to support predictive modeling and early warning for climate-sensitive diseases, with a focus on malaria. Before the launch in March 2024 of the Wellcome-funded DHIS2 for Climate & Health project, led by the HISP Centre at University of Oslo (HISP UiO), there were already two separate local initiatives in Mozambique on climate-informed forecasting of malaria incidence. However, despite some promising outputs, several persistent challenges prevented these models from being put into routine use to guide planning decisions for malaria programs.
In Laos, one early-warning model was tested as a proof of concept for a few climate-sensitive diseases, producing some potentially useful results for dengue but less accurate predictions for diarrheal diseases. However, the proof of concept was not adopted or integrated into the national information system, inhibiting the potential for routine use and decision-making by the Ministry of Health.
To learn from the progress and challenges in Mozambique and Laos, HISP UiO initiated an action research collaboration between local HISP groups and health stakeholders in each country. Through this work, we identified several technical barriers and socio-technical challenges that have hindered the routine use of malaria forecasts, including the barriers to integrating and harmonizing climate and health data, the complexity of bespoke modeling tools, the limitations they impose on testing multiple models, and the challenge of integrating them with national DHIS2 systems that would facilitate their routine use. These learnings have informed HISP UiO’s development of the Chap Modeling Platform, a model- and platform-agnostic open-source tool that enables countries to develop, test, and run multiple models side by side, featuring robust documentation, interoperability support, and seamless integration with DHIS2.
Exploring ongoing modeling efforts in Mozambique
As climate and health is a new domain for the HISP network–and for many of our MOH partners in LMICs–a key objective of the initial phase of the DHIS2 Climate & Health project was to learn from previous country experiences to inform our work and ultimately address key gaps that have limited uptake and scale in countries through robust, open-source technology solutions. Stakeholders from Mozambique had already presented their work with DHIS2 and weather data at the DHIS2 Annual Conference in 2023, so it was a natural place to begin our in-depth research.
As of the start of 2024, there were (to our knowledge) two separate climate-informed malaria forecasting projects in Mozambique. One initiative was driven by the National Institute of Public Health (NIPH). It explored the use of a tailored version of a short-horizon statistical forecasting model provided by WHO TDR/Gothenburg University through the EWARS project with the goal of generating monthly or weekly alerts as part of a routine malaria early warning system, as well as several models developed in-house by NIPH, including a medium-horizon (full-season) forecasting model. The malaria forecasting outputs produced by NIPH using their own software systems were intended to support risk mapping, planning and resource allocation decisions by the NMCP for tailoring malaria interventions. HISP UiO was unable to gain access to the code for these models, making it difficult to assess them or integrate them into our project. Through our research, we also learned that the NIPH models were not integrated with routine health data from Mozambique’s national DHIS2 system–running the models was a manual process done ad hoc–and that the resulting forecasts had not been integrated into routine use by the NMCP.
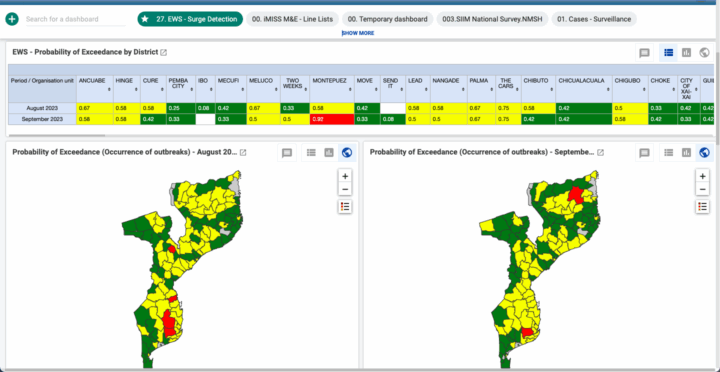
The other initiative was coordinated under the MOH, with technical support from Saudigitus (HISP Mozambique), using a statistical short-horizon forecasting model developed originally by a researcher at the University of Lancaster. This initiative displayed outputs from the model on a DHIS2 dashboard, developed in partnership with the Clinton Health Access Initiative (CHAI). The HISP UiO team explored the MOH/CHAI system through an in-person visit that included meetings with Saudigitus, model developers and relevant stakeholders, as well as an in-depth code review.
In reviewing the code and engaging with the original model developer, several issues became apparent. First, while the model had used climate data at its inception a couple of years earlier, the pipeline for getting climate data into the model had since stopped working, meaning that it was producing forecasts based on historical malaria data alone. Second, the model relied on manual installation in a computing environment that was separate from the DHIS2-based health data infrastructure, and that relied on manual extraction and transfer of datasets from DHIS2 to the model. The complexity of this manual setup severely limited the potential for putting this model into routine use, and the bespoke design of the software as a research project (as opposed to an enterprise-level software tool) made achieving integration with DHIS2 for streamlined data inputs and dissemination of outputs a challenge. As a result of these data integration challenges, the MOH project had not reached a stage where relevant stakeholders had been able to evaluate how well the model worked.
Finally, we also discovered that many technical adjustments had been made to the model’s original code to make it work with the local data formats and computing environment, but that in the years since the original installation the model developer had produced an improved version of the underlying model itself. In order to take advantage of the newer model–or to replace it with a different one, such as a model developed by the NIPH–the team in Mozambique would need to go through the extensive manual work of local adaptation a second time, as would any other country that was interested in adapting this work to their own context.
Learning from the WHO EWARS-csd implementation in Laos
In Laos, the WHO country office and a researcher from the University of Gothenburg had worked with the MOH to test EWARS-csd (a version of the EWARS software that incorporates climate data) as a proof of concept, but had not installed it in the national health information system infrastructure. During the testing process, it became apparent that for the early warning system to function as expected, seamless, automated pipelines from the country’s routine health data sources (in DHIS2) and climate data sources would need to be established.
DHIS2 is already a highly interoperable platform, with well-documented and open REST-based APIs. As a result, DHIS2 is typically able to interoperate with other systems that support a similarly robust (and open) API. DHIS2 experts from HISP UiO and HISP Vietnam (our local partner group that supports the national DHIS2 systems in Laos) had been working with the WHO country office and MOH to attempt to integrate the Laos DHIS2 system with EWARS-csd, but had run into technical barriers that prevented the automation of data exchange between the two platforms, particularly the lack of an API in EWARS-csd. While there was already institutional support for the potential use of the EWARS-csd system in Laos, these technical challenges had prevented it from being taken into routine use.
Insights from action research inform HISP’s approach to developing the Chap modeling platform
Based on our action research with stakeholders in Mozambique and Laos, our observations from the attempts to operationalize malaria forecasting models there, and a literature review on climate-informed malaria and dengue modeling, the HISP UiO team decided to follow a somewhat different approach than the status quo in the climate and health modeling field.
In the standard approach, local customization of existing models is not only limited to tailoring for different priority diseases, modeling inputs and forecasting horizons. It often also requires additional technical fixes to manage differences in computing environments and data formats. This helped inform one central decision by the HISP UiO team: to distinguish the core statistical model from supportive data science functionality like data parsing, evaluation, and results dissemination. Rather than develop a bespoke system built around one specific model, HISP UiO has developed a modularized software platform–the Chap Modeling Platform–that provides a standardized interface into which any statistical model can be incorporated, and where all models can share unified, robust functionality for handling data processing and system interoperability. This supporting functionality can be locally customized independently of model adaptation. The unified interface also allows various models to be evaluated in a rigorous, customizable way, side by side.

Building upon the HISP approach to co-creation of software solutions with country users and generic, reusable and extendable solutions, the Chap modeling platform was conceived to fill a critical gap observed across countries: the lack of robust, modeling infrastructure to accommodate multiple models and facilitating real-time data pipelines from routine data systems like DHIS2. Significantly, as Chap was developed through the DHIS2 for Climate & Health project, which aims to leverage existing DHIS2 systems, data, and local capacity in the 75+ countries where DHIS2 is used at national scale, the Chap platform was designed from the start to integrate seamlessly with DHIS2 both for data input and results dissemination. Taken in combination with the parallel development of the DHIS2 Climate App, which facilitates integration and harmonization of climate data with health data in DHIS2, this effectively resolves the data flow issues encountered in Mozambique.
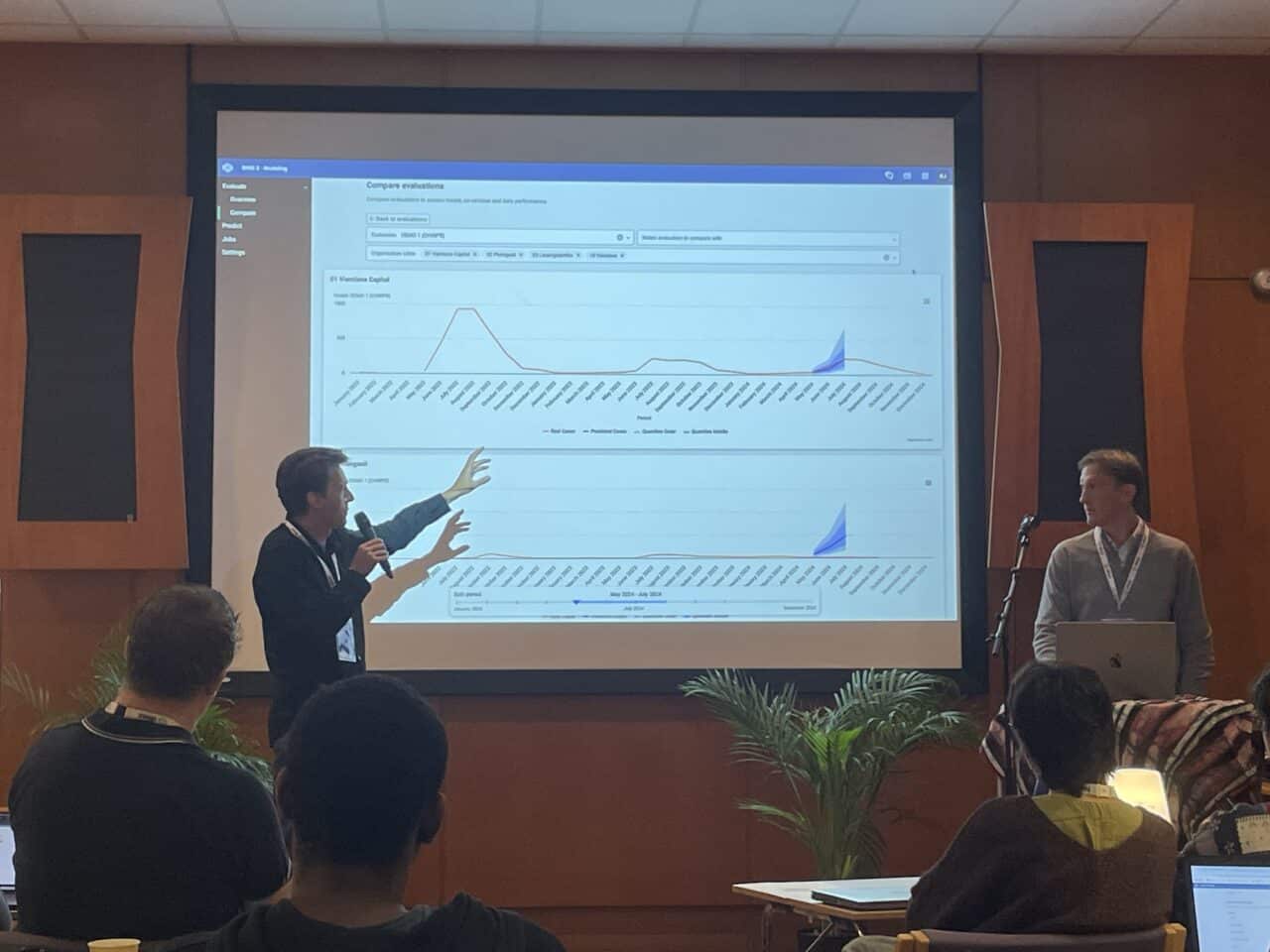
Because it has been built from the start to function within existing national health information infrastructure and routine data streams, the Chap platform enables countries to develop, assess, and run models in an agile way. Using Chap, countries can evaluate multiple models side by side to see which works best for their context, and to see which data sources contribute to improved forecasts. They can also adjust the available open-source models to better suit their context or develop their own, which can then easily be shared through Chap for reuse and adaptation in other countries and contexts.
Recognizing that many countries and stakeholders may choose to use other data platforms than DHIS2, and given the difficulty HISP encountered with lack of interoperability support in the preexisting model solution in Mozambique, Chap was also designed to be platform-agnostic, supporting integration with other data systems and softwares. As Chap is also model-agnostic by design, this means it can serve as shared, generic architecture for model development and testing that countries can use without having to duplicate integration and technical adaptation efforts for each new statistical model they want to try.
In regards to the supportive data science functionality in Chap, the openness of the platform and our direct collaboration with local stakeholders allows the HISP team to see the behavioral needs of each component in its intended context from the outset, helping to ensure that the technical solutions designed by HISP are relevant to local stakeholders and allowing different aspects to be worked on and improved in parallel. Developing data processing and evaluation functionality that is generic to the Chap platform, rather than developed redundantly for each model, allows a broader community to come together to develop more sophisticated and rigorously tested functionality for these aspects. Having unified data handling and evaluation functionality across countries, despite potentially different statistical models being used, promotes experience sharing and facilitates the creation of shared supporting resources, such as training materials, that can also be easily reused and adapted.
Finally, using best practices for open-source software development from the start, including rigorous and generic codebases, software versioning, use of standard solutions like containerization (such as Docker), and thorough documentation on installation, configuration, and use, makes it easier for countries to deploy Chap and keep it updated as the HISP UiO team continues to make iterative improvements to the platform as part of our ongoing action research project. This reduces the time that needs to be spent adapting the underlying software platform, allowing modelers to spend more time working with the models themselves.
This emphasis on openness, iterative co-creation with local partners, and design for adaptability, integration, and reuse is central to the HISP approach, which has guided the work of HISP UiO and the HISP network for the past 30+ years. Applying this approach to the modeling field offers a potential solution to the siloed and bespoke approaches that have limited the potential of countries to put climate-sensitive disease forecasting into routine practice.
Supporting EWARS interoperability with DHIS2
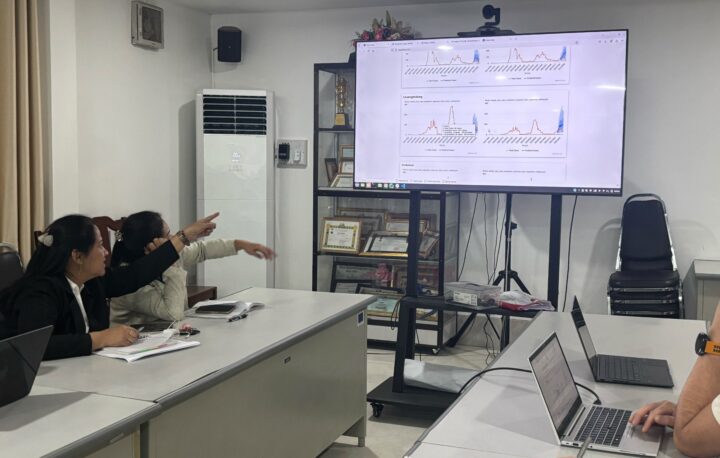
Beyond models themselves, we also recognized in our research that existing tools for climate-sensitive disease forecasting also provide additional functionality that is useful to health stakeholders (such as producing alarms for predicted outbreaks), and that there is already institutional buy-in for their deployment in national health information system architectures. This was the case for EWARS-csd in Laos. The solution we arrived at was not to replace this system, but to facilitate its effective use by streamlining the connection to DHIS2 and Chap.
To achieve this, HISP UiO worked with the University of Gothenburg team to introduce an API for the EWARS-csd system. We worked with the university to test the new API as a means to receive alerts and alarms generated by EWARS-csd as data points in DHIS2 for populating early warning dashboards and generating notifications to health system users.
The development of new code was necessary to facilitate the transformation of data inputs and outputs from EWARS-csd to DHIS2 and vice versa. Ad-hoc scripts for such transformations can be difficult to maintain over time; therefore, HISP UiO made the decision to integrate this code into the Chap platform to facilitate the data transformation needed for EWARS-csd and DHIS2 to be able to send data and information outputs bi-directionally. This offers a streamlined solution for addressing the challenge of managing differences in computing environments and data formats referenced above, and provides a solution that can be adopted by other countries using the EWARS-csd system alongside DHIS2.
Additional lessons learned help guide HISP’s work–and can benefit others in the health modeling field
In addition to informing the development and implementation of the Chap Modeling Platform, HISP’s experiences in Mozambique provided several learnings that we will take forward in our future work on DHIS2 for Climate & Health. These lessons learned may also be useful for others working in the modeling field.
First, when exploring existing systems in countries, it is crucial to have access to the full running code to determine how a solution truly works. For this reason, there is great value in the code being publicly available from the outset, to avoid significant time and effort spent getting access to it. It is also essential not just to have access to the underlying generic model, but also to the adapted code that is actually in use in a given country, as only this will reveal what data is really being used and which specific results are being generated.
Second, even when a model appears to be close to seeing real use, there may be large remaining gaps, both socio-technical and purely technical, to reach true operational use. At a purely technical level, a substantial development effort may be needed to move from scripts running on separate infrastructures with manual data preparation and results dissemination to a solution that can be run regularly on routine data streams with streamlined dissemination of results to relevant stakeholders. On a socio-technical level, it is important to validate models with local stakeholders to ensure that the results are relevant, meaningful, accurate, and usable, and to investigate existing workflows, SOPs, and dissemination channels to ensure that once an early warning system is ready for routine use that there is sufficient buy-in, trust, and organizational support to facilitate the use of its outputs.
Finally, we note that the divide between institutions and ownership and use of data that we observed in Mozambique is a recurring theme in other countries, especially those that have both a Ministry of Health and a National Institute of Public Health. In Mozambique, HISP found that the MOH is the owner of the country’s malaria data–and the health agency that is empowered to act on this data–while the NIPH provides data analysis services to answer discrete policy questions or to support specific projects and initiatives. The gaps between these organizations, which may be both technical and socio-technical, can make it challenging for a malaria programme in a Ministry of Health to operationalize ad hoc analyses and forecasts produced by a National Institute of Public Health. Encouraging both agencies to use a shared modeling platform, such as Chap, could be one avenue toward addressing this challenge.
Learn more about Chap and the DHIS2 Modeling App with this presentation from the 2025 DHIS2 Annual Conference: