Integrated Human Resources for Health using DHIS2 and FHIR in South Africa
DHIS2 serves as a platform to extend effective data warehousing and analysis for human resource planning through integration and interoperability
Functional health systems depend on a number of inputs to be effective, including good facilities, adequate equipment and efficient logistics systems for commodities. One key input is skilled health workers, also known as Human Resources for Health (HRH). The Global Strategy on Human Resources for Health report, published by the WHO in 2016, projected a worldwide shortfall of 18 million health workers by 2030, with most of the shortfalls in low and middle-income countries. South Africa’s Ministry of Health, with the support of HISP South Africa and other partners, has taken steps to address this looming crisis by developing an integrated HRH system that leverages modern technologies – including DHIS2 and FHIR – to identify HRH needs in its health systems and plan to address them. With the onset of the COVID-19 pandemic, this system was put to the test. Enhancements made during the pandemic helped South Africa respond to this crisis, and planned future developments can help the country reach its Universal Health Coverage goals.
Impact of the COVID-19 pandemic on HRH: protecting and treating health workers, and managing staffing shortages
When the COVID-19 virus became a threat to global health in early 2020, health care managers in many countries faced a plethora of challenges, ranging from limited understanding of the virus’s transmission modes to managing mass hysteria among the populace. These challenges stretched the healthcare systems in most countries beyond their normal limits. To tackle these issues, healthcare managers had to rely not only on established frameworks for epidemic response but also devise new solutions to slow the exponential spread of the virus, with its attendant rising morbidity and mortality.
Frontline healthcare workers felt a significant impact of the pandemic in its early days. While scientists raced to develop a vaccine and administrators frantically tried to procure sufficient Personal Protective Equipment (PPE) for the medical staff, many essential healthcare personnel got infected and hospitalized. The situation was further worsened by severe equipment shortages, lack of enough hospital and ICU beds and a general breakdown of the global supply chain. This chain of events presented a unique situation in which healthcare administrators needed to deploy the increasingly declining workforce more efficiently to care for vulnerable populations while nursing other affected health workers back to health so they could join in the efforts to contain the pandemic. Healthcare administrators the world over relied on data-driven systems to ensure effective deployment of scarce specialized personnel to prevent a total collapse of the healthcare systems.
In Sub-Saharan Africa, many countries faced these same challenges, but to an even greater degree given the prevailing shortage of qualified staff. For example, the doctor-to-patient ratio within the sub-region averages about 1:5,000 which is a far cry from the WHO recommended ratio of 1:600. The need for efficient deployment of healthcare professionals using systems that leverage accurate and readily accessible data could not be over-emphasized.
South Africa’s robust HRH system supports Universal Health Coverage goals and helps respond to COVID-19
As was the case in many countries, frontline health workers in South Africa were among the most affected by the virus. The rising number of infected health workers constituted a burden on the workforce, threatening to derail an effective response to the pandemic and other healthcare needs in the country.
The pandemic immediately highlighted some HRH planning challenges, which included the identification of specialist doctors, ICU qualified specialist staff, calculating PPE requirements and identifying where these PPEs should be sent. In February 2021, when the country received its first batch of the COVID vaccines, the South African National Department of Health (NDoH) prioritized healthcare workers among the groups to be inoculated to strengthen the country’s efforts at combating the virus. All health workers including those outside the public sector needed to be identified so that the country could estimate the number of vaccines required to protect healthcare workers throughout the country; and where the vaccines were more urgently needed. Fortunately for South Africa, the country’s health administrators had a head start.
In 1997 when South Africa developed the White Paper for the Transformation of the Health System, HRH was emphasized as one of the key drivers of the mission to bolster the country’s health systems. Building on that, the NDoH developed its strategic policy guideline document in 2011 to direct investments and coordinate activities geared towards ensuring a sufficient, competent and empowered healthcare workforce for South Africa. Subsequently, the guideline helped the country develop a robust HRH registry and the NDoH Human Resource Information System (HRIS). Also, as part of its commitment to achieving Universal Health Coverage (UHC) by 2030, in line with the declarations at the UN General Assembly meeting, the South African government, through the NDoH, formalized the 2030 HRH Strategy. The tenets of the strategy include the following:
- Effective health workforce planning to align with current and future needs.
- Institutionalize a data-driven and research-informed health workforce policy, planning, management and investment.
- Produce a competent and caring multi-disciplinary health workforce through an equity-oriented, socially accountable education and training system.
- Ensure optimal governance, build capable and accountable strategic leadership and management in the health system.
- Build and enable a productive, motivated and empowered health workforce.
Leveraging DHIS2 and FHIR to interconnect data sources into an Integrated HR Information System
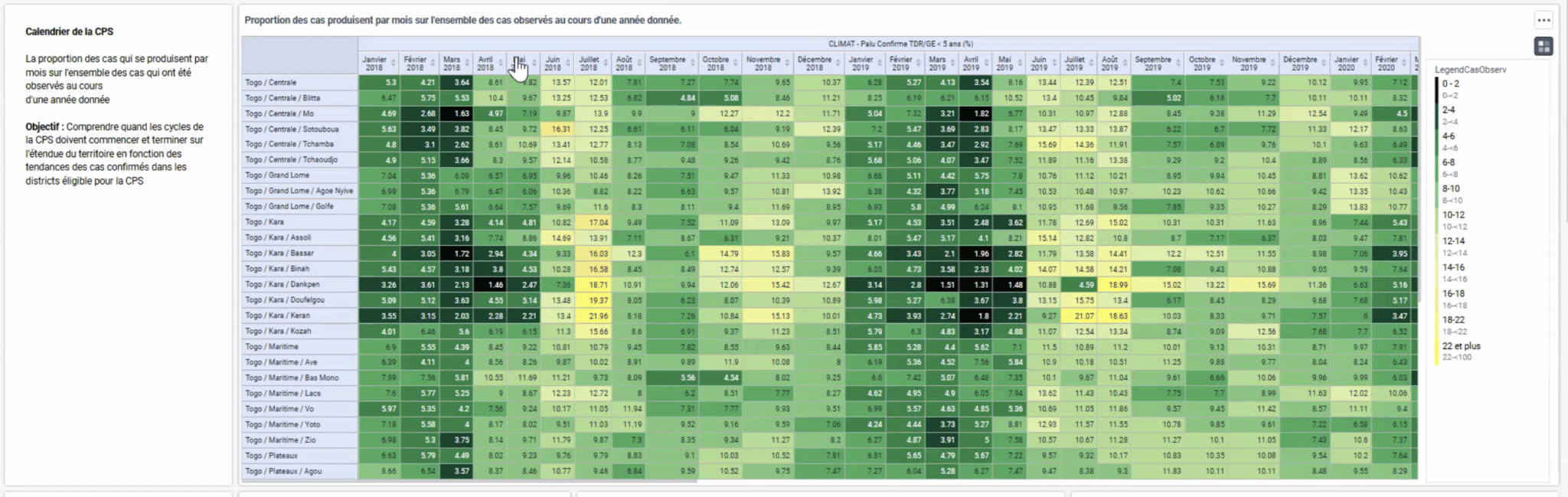
The NDoH maintains a robust digital HR registry built based on the Fast Healthcare Interoperability Resources (FHIR) format using the mCSD IHE profile. FHIR is an open-source standard that supports the easy transfer of healthcare data in the Health Level Seven (HL7) format across systems. The HR registry receives data inputs from multiple primary sources including a government payment system, health professions regulatory councils and the private sector, in various data formats. Data from these sources are parsed through a staging system for cleaning, automation and the Extract, Transform and Load (ETL) process before being aggregated into the HR registry. The ETL process combines data from multiple sources into a single and consistent unit before it is transferred into the HR registry using Apache Airflow, an open ETL software. As of early 2022, the registry holds over 1 million records and is the authoritative repository of demographic information on healthcare workers in South Africa. It is also the first component of the integrated HRIS.
The next component of the HRIS is the data warehouse built on the DHIS2 platform. Data in the HRH registry are imported into the data warehouse, where aggregated HR data are built into customizable dashboards providing immediately accessible and actionable information for HR planning and reporting, such as health workforce by cadre, which was used to identify where vaccines needed to be sent first during the vaccination campaign and in identifying ICU-trained staff to redeploy. As the home of the original HISP program and site of the development of version 1 of the DHIS software, South Africa leverages decades of DHIS2 experience and local capacity to enable effective use of DHIS2 HRH data.
South Africa’s HRH system also takes advantage of the extensive interoperability capabilities of DHIS2 to integrate other solutions. This was achieved by building a mesh of connected APIs. The HRH API mesh facilitates data exchange with the National COVID Data Lake, a system that collects information about health workers infected with the virus. The system also connects to the National Vaccine eRegistry for the country to determine health workers eligible for the COVID vaccine. This system, among other factors, helped South Africa achieve a high COVID-19 vaccine coverage for its health workers in a short time frame when compared to other Sub-Saharan African countries. By the end of 2021, 59% of healthcare workers in South Africa had been vaccinated, compared to only 1 in 4 healthcare workers in Africa overall.
Reporting of different dimensions of the HR data, like the number of doctors per 10,000 population, is done with records pulled from a separate instance of DHIS2 through the DHIS2 API. Additional granular reporting is achieved with business intelligence software such as Superset. These reports are routinely published on the HRH web portal which acts as a unified point of access to the HRH information. The DHIS2 reporting features also make it easier for the NDoH to measure some WHO indicators such as HRH coverage for different health specialties at the national and sub-national levels. These reports help the NDoH to track progress towards achieving the goals outlined in the 2030 HRH Strategy and ultimately, UHC for all South Africans.

Finally, the last component of the integrated HRIS is the HR Planner module, a custom Machine Learning (ML) application being developed by HISP South Africa with the support of the U.S. Centers for Disease Control and Prevention (CDC). This app is aimed at facilitating HR planning to meet current and future needs. It is a data-driven scenario simulation system that would enable health managers to plan effective health workforce management for hypothetical scenarios such as wartime and disease outbreaks as well as routine operational needs. Results from these analyses will guide national and regional budgeting for the training and deployment of additional health workers of specific specialties to maintain a good level of preparedness and response to healthcare needs and to achieve UHC.
Next steps for South Africa’s HRH system: Improving data quality, leveraging machine learning, and refining analytics outputs
To gain additional utility from the system, plans are in motion to further enhance the system by improving data quality in source systems. The HR planning module is still being developed to facilitate future planning by utilizing machine learning and predictive analytics modeling. Furthermore, additional analytics outputs and reporting are proposed to help HRH managers at all levels gain better insights and use available data for better planning. These efforts will ultimately help the NDoH achieve the 2030 HRH strategic goals.
South Africa’s integrated HRIS is a product of good planning and excellent execution by the NDoH in collaboration with its partners including the CDC and HISP South Africa. It has so far helped the country improve efficiency in its HRH needs at such a critical time as the ongoing COVID pandemic. Health managers in the country have taken advantage of the interoperability features of DHIS2 and the FHIR standard to expand the capabilities of their HR systems and fast-track their efforts to achieve Universal Health Coverage.
To learn more about this project, read a detailed description on the DHIS2 Community of Practice and watch a presentation by HISP South Africa from the DHIS2 Annual Conference.