The DHIS2 Annual Conference takes place from 15-18 June 2026! Learn more
Improving Treatment Adherence for Multi-Drug Resistant Tuberculosis in Uganda Using DHIS2
The Ugandan Ministry of Health’s DHIS2-based electronic Case-Based Surveillance System (eCBSS) helped to increase linkage to second-line TB drugs from 66% to 98%
According to the WHO, Tuberculosis (TB) is the world’s second-deadliest infectious disease. Uganda has a TB prevalence of 253 cases per 100,000 population. This puts the country among the world’s 30 high-burden countries, with about 3,500 new cases every year and a total incidence of 91,000 cases. Two out of every 100 TB-infected people in Uganda have drug-resistant TB (DR-TB) and require second-line drugs to improve their outcomes. DR-TB typically develops in TB patients who have abused their TB treatment drugs or who do not complete their treatment as prescribed. These new strains of DR-TB bacteria could also spread and infect new patients who also develop resistance to treatment. DR-TB is also quite expensive to treat at the rate of about $1,200 per patient in Uganda.
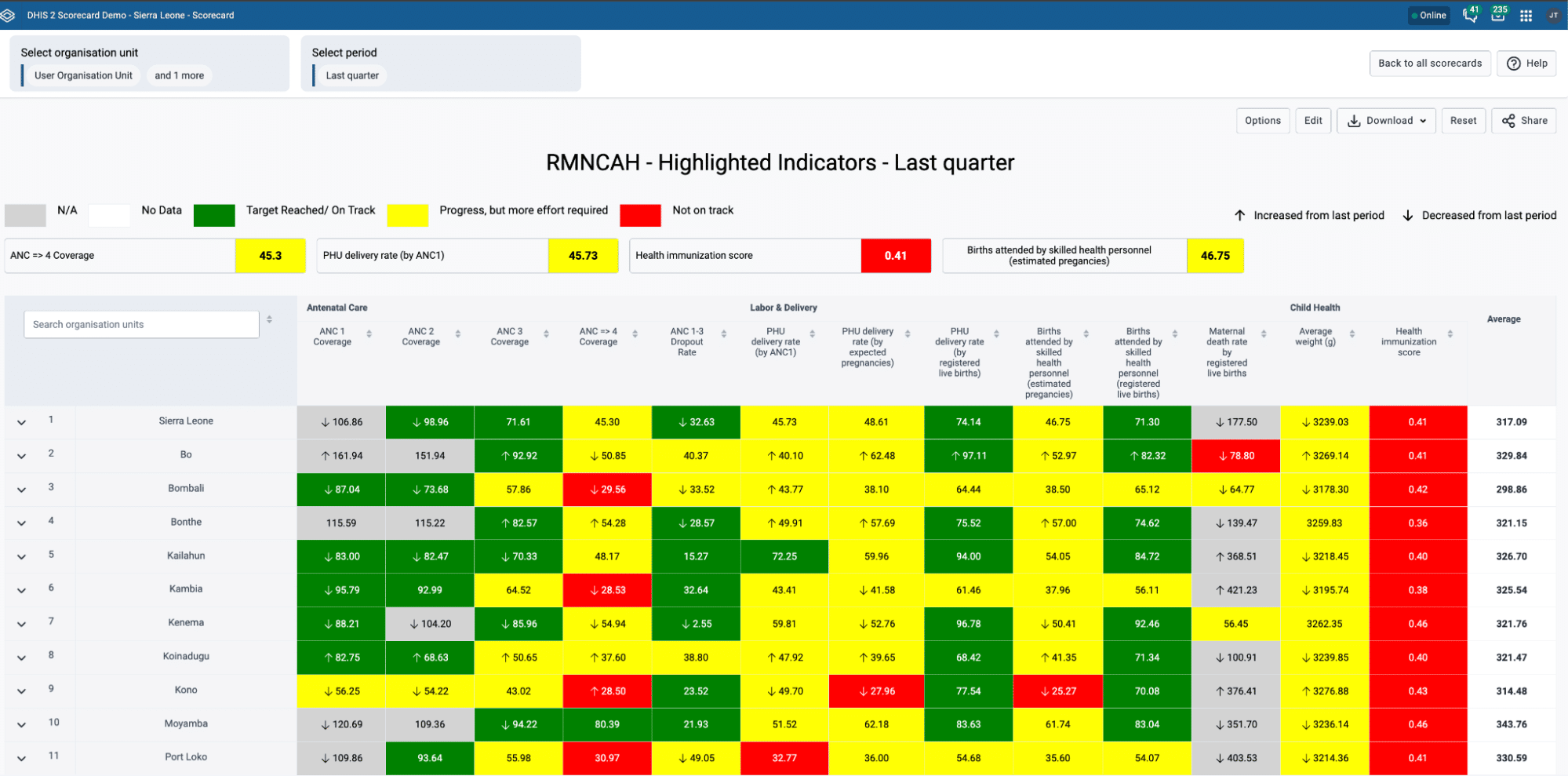
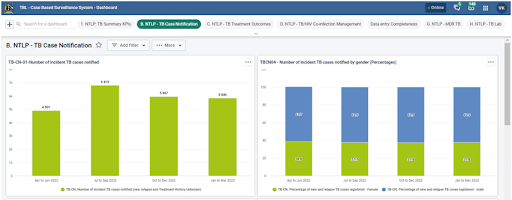
In 2020, the Ministry of Health (MoH) in Uganda implemented an electronic case-based surveillance system (eCBSS) based on DHIS2 Tracker to report and monitor the linkage of TB patients to second-line drugs. Uganda has been reporting aggregate TB data from across all health facilities into DHIS2 since 2012, while information on DR-TB cases was collected on paper forms. Data quality challenges, limitations of manual data collection methods, as well as the need to improve linkage to treatment services and attain a high treatment completion rate prompted the MoH to adopt Tracker for case-based surveillance. In 2017, the HISP Uganda team implemented a small-scale Tracker system called Drug-Resistant Tuberculosis Health Management Information System (DRIMS), to collect DR-TB data, beginning with the national center, before scaling it up to all 18 DR-TB sites by 2019. Though the DRIMS solved some of the data quality challenges, it was limited to a few visualizations and recorded data on DR-TB only. Consequently, the MoH implemented the eCBSS which captures expanded data on laboratory confirmation, DS-TB, DR-TB, leprosy and contact tracing. Existing patient data in DRIMS from all DR-TB treatment sites were migrated into the eCBSS. The Tracker-based eCBSS was configured with the support of HISP Uganda and has been rolled out in 504 of the 1,810 TB Diagnostic Treatment Units in the country, including all 18 multi-drug resistance (MDR) treatment sites.
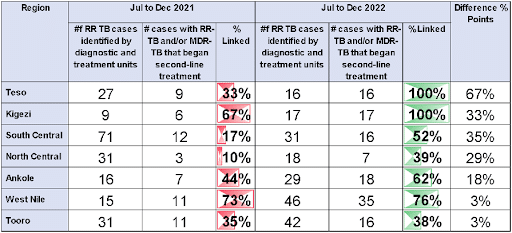
Since the eCBSS was implemented, second-line drug linkages have improved due to better access to patient-level data. The percentage of patients who were linked to second-line treatment throughout the country increased from 66% between July and December 2021 to 98% during the same period in 2022. Three out of all 29 districts made significant contributions to this increase over the period. Teso Region increased linkage from 33% to 100%; Kigezi, from 67% to 100%; and South Central, from 17% to 52%. Furthermore, the eCBSS has reduced the delays in linkage to treatment by notifying treatment sites with relevant contact information (e.g. telephone number, address and next of kin) for patients with DR-TB in customized dashboards once the cases are confirmed in the laboratory. Contact tracing, adherence to treatment and management decisions have also been enhanced by the eCBSS.
(Using DHIS2 Tracker) we are able to account for the people who have DR-TB–who they are, where they’re from–and do much more. We can do geographical or spatial analysis… We can know the hot spots. And this has really been due to the Tracker-based DHIS2. It was a magic bullet.
Transitioning to an electronic surveillance system to improve treatment outcomes
Prior to the implementation of the eCBSS, DR-TB case records were collected manually, using paper-based forms. The records were also manually tallied and reported as aggregate data to higher levels through the routine Health Management Information System in DHIS2. However, this method presented data quality issues including errors from inaccurate patient management data and transcription errors, especially during manual tallying of records. Also, the paper-based system for data aggregation was time-consuming, did not support real-time data analysis and restricted in-depth investigations for better management decision-making. In view of these, the MoH found the need to improve DR-TB case detection, linkage to treatment and to ensure that patients complete their regimen. With the support of HISP Uganda, the MoH implemented the eCBSS and began tracking DR-TB using the platform in 2020.
The team started rolling out the eCBSS at the DR-TB treatment sites which already had a DHIS2-based digital management information system (DRMIS). The case-based surveillance system would strengthen information management at those facilities and help them make better data-backed decisions. The DR-TB focal persons at the treatment sites use patient data, now available in real-time Tracker line lists, to contact confirmed DR-TB patients directly for immediate initiation into appropriate treatment and to ensure the patients complete their treatment. They also rely on the Tracker data to start contact tracing with the view to identifying index cases and curtailing further transmission of the disease. Subsequently, the system was rolled out to other health centers and hospitals across the country. Furthermore, the roll-out process was accompanied by extensive training of different categories of health workers including 1400 clinicians, 527 records assistants and stakeholders to ensure optimum utilization of the system. The training also included district biostatisticians who help with analyzing data at the district level.
Integrated workflow and routine monitoring for effective data use
Persons with suspected TB infection in all entry points of the health facilities, including The Out-Patient Department (OPD), Antenatal, and In-Patient, are screened using the intensified case finding form. From these entry points, patients who have been presumed to be infected with TB are entered into the presumptive TB register before confirmatory tests are conducted in qualified laboratories. If the test results return positive for TB, the patients’ records are then entered into the eCBSS which in turn, generates and sends notifications in SMS formats to the assigned DR-TB treatment site. The identified case(s) are also reflected on custom DHIS2 dashboards immediately, making the data available to healthcare managers at the district and national levels for prompt action. Standardized quick follow-up actions are immediately initiated by the TB or DR-TB focal person for the site to ensure that the patient(s) are started on treatment in the shortest possible time. This will often require the focal persons to contact the test facility and the patient by phone and make proper arrangements to get the patient over to the treatment units for the immediate commencement of the proper regimen.
Additionally, the eCBSS generates appointment lists for each patient, which the focal persons use to schedule and track patients’ visits until treatment is complete. When a patient misses a scheduled appointment, personal contact information collected in Tracker helps the focal persons reach out to the patient and convince them to return to treatment. This helps improve treatment adherence and outcomes.
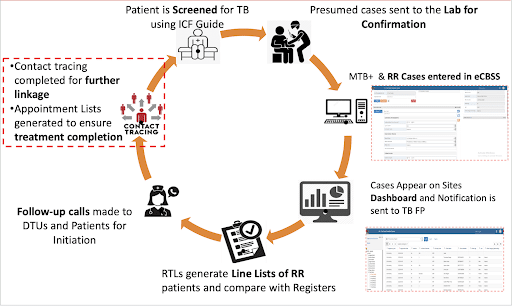
Also, the management team conducts weekly routine data quality monitoring exercises. This is done by comparing the data entered in the eCBSS with what is in the manual records or the hard copy reports to ensure concurrence. Where there is any difference in data recorded on Tracker with what is on the paper registers, the discordance is investigated and the error quickly corrected to maintain high data quality for decision guidance. This weekly review which is conducted by the regional TB and leprosy supervisor further strengthens treatment linkage by identifying any missed case and following up with phone calls. The eCBSS system has also helped Ugandan health authorities identify geographical “hot spots” or clusters of DR-TB cases. By going on-site to perform contact tracing in these areas, the team was able to identify more cases of DR-TB, helping to get those additional patients started on treatment programs more promptly.
Another important way the MoH in Uganda has utilized improved data facilitated by Tracker was to encourage peer review and support. Available data in eCBSS show that some regions have improved treatment linkage much better than others since its implementation. TB program managers are using this data to identify focal persons who are behind the recorded successes, especially those who have achieved 100% linkage within a specific time frame, and encouraging them to share their approaches and key lessons so that other regions can learn from those and improve their own output.
Scale-up plans: Equipment integration and artificial intelligence for deeper insights
The eCBSS has improved many aspects of the TB program in Uganda, including data quality, treatment linkage timeline, patient follow-up, contact tracing, and better management decisions. Nonetheless, the team is keen to further enhance the capabilities of the system to facilitate integration and interoperability with other systems in all diagnostic and treatment units. The team plans to integrate the eCBSS with EMR and point of care systems, especially the already existing HIV EMR, thereby eliminating the need for manual data entry in the eCBSS and the attendant chance for transcription errors. Also, plans are underway to integrate the system with relevant diagnostic equipment like the GeneXpert machine such that DR-TB cases would be recorded in Tracker, directly from the testing machines once they are detected, for case-based surveillance.
Finally, the team is exploring how to integrate artificial intelligence and machine learning with case-based surveillance for MDR-TB patient management. It is believed that this will further optimize the eCBSS and generate better insights to guide decision-making toward DR-TB elimination in Uganda.
This article is based on a presentation given by Vincent Kamara, Data Manager, National TB and Leprosy Control Division, Ugandan Ministry of Health, at the 2023 DHIS2 Annual Conference. Watch the presentation and a follow-up interview on the DHIS2 YouTube channel.