The DHIS2 Annual Conference takes place from 15-18 June 2026! Learn more
DHIS2 and Electronic Medical Records
As a native digital health registry, DHIS2 is a viable option for a lightweight EMR to support primary healthcare delivery. Explore the built-in features of DHIS2 that support facility-level collection and management of patient records and other longitudinal health data
Jump to a section on this page
What are Electronic Medical Records?
There are a number of different approaches to collecting and managing health information on individual patients and clients. Before discussing the role of DHIS2 in this space, we will review some commonly used terms and discuss the purposes they serve and functionalities they each are intended to provide. In drafting the working definitions below, we have drawn on authoritative sources where possible, while acknowledging that the boundaries between these terms are not always clearly defined or universally agreed upon.
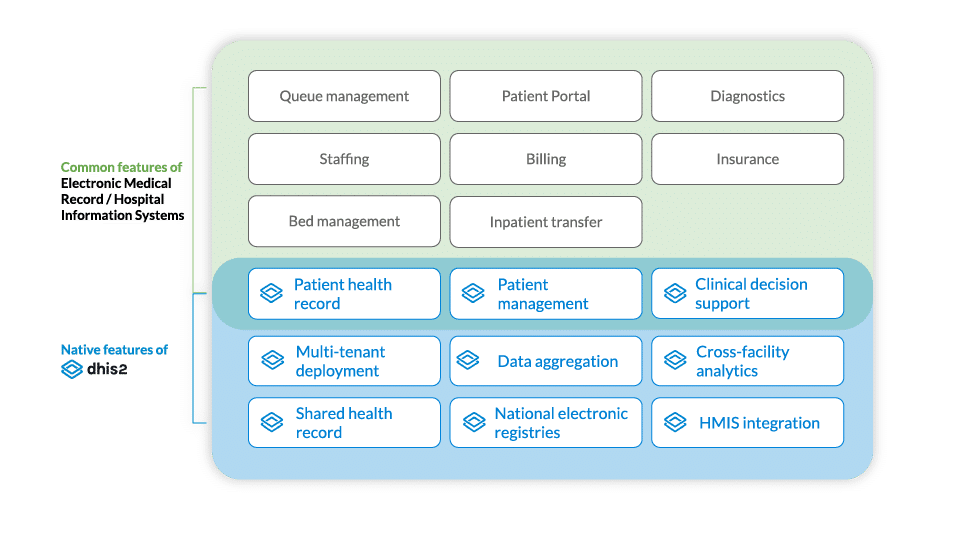
- Electronic Medical Records (EMRs) function as digital versions of a patient’s file, containing their medical and treatment history. EMRs are used to manage patient information like diagnoses, medications, and lab results. They can be accessed and updated by users across departments within an organization, such as different units within a hospital, and often include decision-support and automation features that can improve workflow efficiency and patient care. Frequently, EMRs are also expected to support insurance, billing, and payment workflows, and sometimes other features (e.g. queue management, bed management) that more properly belong to Hospital Information Systems, described in detail below. EMRs do not necessarily provide native support for data aggregation and analysis across multiple organizations or levels within a health system.
- Hospital Information Systems, also known as Hospital Management Information Systems, are software platforms that manage all operational processes in a hospital, such as patient records, laboratory and radiology results, appointment scheduling, bed management, billing, and financial transactions. They aim to streamline hospital operations by digitalizing them within one platform. EMRs can be understood as one component of a Hospital Information System.
- Electronic Health Records (EHRs), also known as Shared Health Records, are digital systems that are designed to collect and manage longitudinal data on individual patients that can be shared across facilities. While an EMR is typically used within one healthcare organization (e.g. a single hospital), EHRs bring together information on patients and populations from multiple organizations, with EMRs serving as a key data source. EHRs can thus provide a more holistic view of a patient’s health history and facilitate analysis at the population level.
- Digital Health Registries, also known as eRegistries or Trackers, are systems for collecting and managing health data electronically, often used for public health surveillance and patient care. They provide digital records for individuals on one or more health programmes, such as testing and treatment for specific diseases (TB, HIV, malaria, etc.), vaccinations (e.g. Electronic Immunization Registries ), or maternal and child health. Alternatively, registries might also serve as a master patient index to link unique records across registries.
DHIS2 as a platform for patient-level data
While best known as a platform for collecting and analyzing aggregated health data for population-level analysis and planning–as a Health Management Information System (HMIS) or national health data warehouse–DHIS2 is also widely used for managing individual-level patient and client data. Through DHIS2 Tracker programs, Ministries of Health and other organizations can easily collect and manage key information for individuals for one or more health programmes over time.
In the sections below, we explain how DHIS2 can be used as a digital registry, as a shared health record/EHR, and as a facility-level EMR for primary healthcare. It is important to note that due to the flexible, modular nature of DHIS2, these do not need to be thought of as separate systems–they can each be employed within the same national DHIS2 architecture, and deployed at different scales and in different geographies or contexts depending on the needs of the health system and the country’s readiness for individual-level data collection based on its DHIS2 maturity profile. This means that countries can use DHIS2 to begin collecting patient data in a limited way (such as for high-priority programmes or targeted districts) and then build up their system over time without the need to replace the underlying software platform.
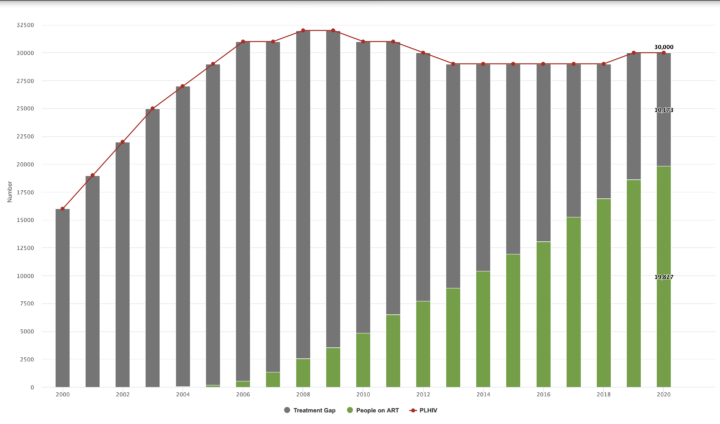
Using DHIS2 as a digital registry
Digital registries built on DHIS2 have proven effective in achieving results for high-priority health interventions–such as helping to reduce vaccination dropout rates and improve TB surveillance and HIV treatment adherence. When implemented in DHIS2, these systems also benefit from several key EMR-like features–including decision support, automated patient messaging, and longitudinal records. Registries implemented in DHIS2 also benefit from robust features for automating the aggregation and analysis of individual-level data, allowing seamless integration with the HMIS for routine reporting and analysis of key indicators.
The use of DHIS2 as a digital registry is well established. DHIS2 is listed by GovStack as a Digital Registry “Building Block” software tool, supporting Digital Public Infrastructure (DPI) approaches for individual-level data management in the health sector and beyond. More than 80 countries around the world use DHIS2 to manage individual patient or client data for one or more health programmes, with hundreds of millions of individual records in DHIS2 systems worldwide. Some countries, such as Palestine and the Maldives, have combined numerous programme-specific Tracker modules together into one holistic system for electronic patient records in DHIS2.
Using DHIS2 as a shared health record/EHR
By deploying DHIS2 as a Digital Registry/Tracker or lightweight EMR, countries can also leverage its robust data management and analysis features to use DHIS2 as a shared repository, which is supported by DHIS2’s default role as a centralized national registry. DHIS2 can also serve as an EHR/shared health record within a larger health information system architecture, allowing countries to bring together individual health records and data from a range of EMRs, including EMRs that are deployed using other software solutions. In scenarios where there are many kinds of EMRs/Trackers in use in one country, DHIS2 can thus provide a unified platform in which data from these siloed systems can be analyzed holistically–including linking individual patient data with routine health data in the national HMIS–providing health stakeholders with better oversight and ability to analyze and respond to health trends.
Using DHIS2 as a facility-level EMR for primary healthcare
Using DHIS2 as a lightweight or “mini” EMR at primary care level offers several advantages – particularly in contexts where full EMRs are impractical due to cost or infrastructure limitations. Because such systems can be built within existing DHIS2 infrastructure–and because it is deployed as a multi-tenant system, with one central instance serving multiple health facilities, unlike EMR solutions that must be locally deployed at each facility–Ministries of Health can introduce longitudinal patient records and EMR-like functionalities at the point-of-care without the heavy costs and delays associated with deploying EMRs at scale. They also benefit from DHIS2’s proven design for low-resource settings—supporting offline mobile data capture and native aggregation of patient-level data into national systems. Moreover, DHIS2’s interoperability and extensibility allow for additional EMR features through custom apps or integration with other platforms.
Despite these advantages, it should be noted that DHIS2 was not specifically designed to support the full range of EMR functionalities. It lacks key functionalities required by larger hospitals and inpatient facilities, such as billing, insurance, and diagnostic workflows; patient portals, appointments, and queueing; as well as staffing and bed management (though some of these can be covered to a limited degree using basic DHIS2 forms). DHIS2’s role as a pragmatic, lightweight EMR can help to overcome traditional barriers to digitizing patient data at the primary healthcare service delivery level, while also enabling interoperability and integration with more comprehensive EMR software established at hospitals and other secondary/tertiary care levels.
EMR features & functionalities in DHIS2
The DHIS2 platform includes built-in functionalities that fulfill key requirements of facility-level EMRs, EHRs, and digital registries:
Person-centric data management
- Capture essential patient data including biographical information and ID numbers, diagnoses, lab results and any other data relevant to your context using fully customizable forms.
- Manage longitudinal patient records to track key information or monitor progress through one or more health programs over time.
- Link records for related clients, allowing you to connect records where appropriate, such as for a mother and child.
- Transfer client records between facilities to reduce duplicate entries and support holistic patient care.

Frontline data capture & validation
- User-friendly data entry on mobile devices or web browsers for both real-time and secondary data entry.
- Robust offline mode for data capture, supporting use in areas with limited internet connectivity.
- Automatic data sync with the central DHIS2 database, enabling real-time monitoring
- Built-in data validation through customizable logical rules and data quality checks.

Decision support & automation
- Customizable workflows based on programme-specific requirements, which can provide basic decision support.
- Dynamic form logic to simplify data entry and reduce errors.
- Automated notifications including SMS and emails to health workers and/or patients based on customizable criteria.

Reporting & analytics
- Dynamic working lists to support effective planning, monitoring, and follow up.
- Built-in reporting features provide an overview of key data on a facility’s patients and services.
- Data visualization & mapping through built in DHIS2 analytic tools, including tables, graphs, maps, and dashboards.
- Seamless aggregation of individual-level data into the national HMIS to facilitate calculation of key indicators and population-level analysis.

Privacy & security
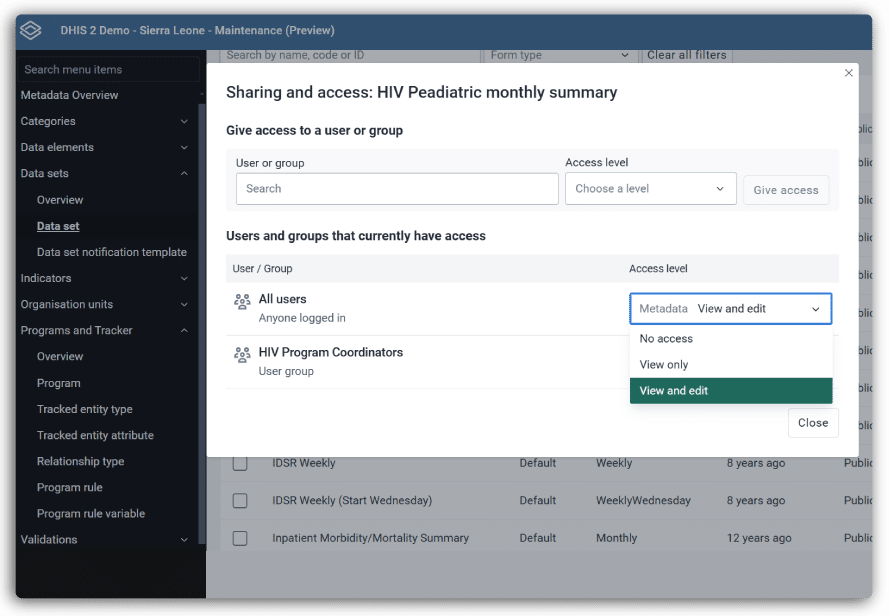
- Role-based access control to limit risks of improper access to personal data.
- Mobile database encryption to prevent unauthorized access to data on mobile devices.
- Compliance with privacy standards: DHIS2 provides the tools to implement systems that comply with GDPR, HIPAA, ISO-27000 and other standards.
Add extended functionality
- Extensibility by design through native support for custom plug-ins and applications, allowing you to add the features you need directly in DHIS2
- Connect to national ID registries such as CRVS systems and digital identity platforms to support holistic, patient-focused management
- Standards-based interoperability with support for FHIR and common data standards such as SNOMED GPS, LOINC, and ICD-10/11

DHIS2 interoperability & integration to support unified information architectures
DHIS2 is designed with interoperability in mind, supporting data exchange through various formats via the open DHIS2 API–including support for common data standards such as FHIR–to facilitate a cohesive health information ecosystem. It integrates seamlessly with several established open-source EMR platforms (such as OpenMRS, OpenEMR, and Bamhni) and complementary national systems such as Civil Registry and Vital Statistics (CRVS) systems, lab information systems and master patient indices. It can be extended to connect with external digital tools that support functionalities like biometrics and advanced diagnostics. This helps countries reduce fragmentation and supports the creation of unified information architectures for patient data.
Impact stories: DHIS2 for electronic patient records
Here are some examples from a selection of countries that show how using DHIS2 for electronic patient records can make an impact on program efficiency, effectiveness, and cost.
You can also read additional articles and published research about the role and effectiveness of DHIS2 for patient-level data management:
- Implementation of an HIV Case Based Surveillance Using Standards-Based Health Information Exchange in Rwanda
- Cervical Cancer Screening Data from the Case-based National Electronic Registry in Bangladesh
- Challenges and Opportunities in Digital Screening for Hypertension and Diabetes Among Community Groups of Older Adults in Vietnam: Mixed Methods Study
- The feasibility of utilizing district health information system and short message services on decreasing child immunization dropout and increasing vaccination timeliness in Duhok Governorate
Presentations & Webinars
Watch these informative webinars and presentations for useful guidance, lessons learned, and best practices.
Navigating the Health Information System (HIS) Landscape
A webinar by the Global Financing Facility that explores the different types of Health Information Systems (HIS) and explains how each type of system addresses different data use needs.
Tracker for Health
This session from the 2024 DHIS2 Annual Conference includes a discussion on how DHIS2 supports EMR use cases and real-world examples from Iraq, Somalia, the Maldives, and Palestine.
Tracker for Clinical Use & Supervision
From the 2022 DHIS2 Annual Conference, this session explores the use of DHIS2 Tracker programs at the point of care in locations which have never had a digitized tool before.
Resources & Documentation
Get started with DHIS2 for electronic patient records with these helpful resources:
Documentation
The Tracker Implementation Guide contains useful information about planning and implementing DHIS2 systems for patient-level data.
DHIS2 Health Data Toolkit
Find useful resources and downloadable metadata to help you configure DHIS2 for patient-level data in key health programmes.
DHIS2 Maturity Profile
A tool for assessing a country’s readiness for implementing DHIS2 systems at different scales and levels of complexity.
Developed in collaboration with local and global partners
The DHIS2 functionalities and features that support patient-level data management have been developed in response to the needs of countries in the Global South, and in direct collaboration with local stakeholders, as part of HISP UiO’s mission of supporting information system strengthening in LMICs.